The 7 Habits
Routines, Risk, and Radiographs: Building a Framework for Stress-Free Implant Dentistry
The Seven Habits of Highly Effective Implant Dentists (Sort Of)
Why Protocols Reduce Stress—And Improve Outcomes
One of the best ways I’ve found to reduce stress in clinical practice is to build routines and protocols for the day-to-day stuff. That way, when things get challenging, it’s more fun than frantic.
I’m not talking about becoming an automaton—carrying out treatment without thought or nuance. I mean having a framework that reduces the number of decisions you need to make on the spot. It frees up cognitive space for the real challenges.
Stephen R. Covey’s The Seven Habits of Highly Effective People is one of the best reads for any professional. You’ll hear people refer to its principles in everyday conversation. Dentistry isn’t so different. So I’ve borrowed the title—loosely—to outline the habits I believe every implant dentist should adopt.
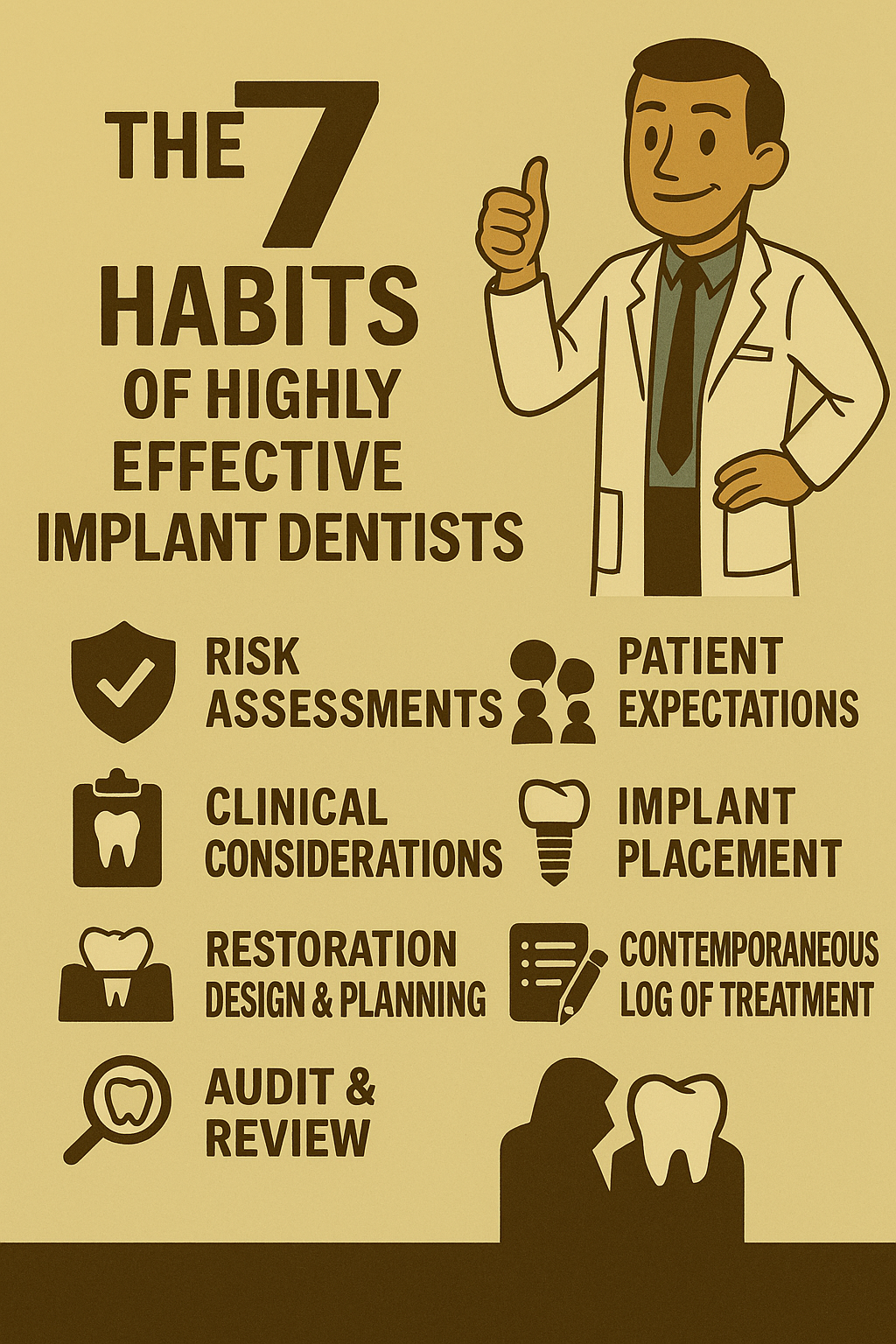
The Core Principles of Implant Care
Let’s call these the “seven-ish” habits:
- Risk Assessments
- Patient Expectations
- Clinical Considerations
- Implant Placement
- Restoration
- Design & Planning
- Contemporaneous Log of Treatment
- Audit & Review
Okay, I know that’s not exactly seven—but close enough.
Habit 1: Risk Assessments Should Be Methodical
I use a custom screen on Exact. And no—it’s not prefilled. Every data field must be clicked for a response, or it stays blank. Atul Gawande’s The Checklist Manifesto was clearly written with me in mind.
If you don’t have a custom screen, the ITI’s SAC assessment tool is a good start. It’ll give you a sense of case complexity and can be saved as a PDF in the patient’s notes. But remember: complexity is just one piece. A comprehensive assessment of patient expectations and clinical considerations is essential. If you’re unsure what that means, the ITI has excellent CPD resources.
Habit 2: Plan from the Final Restoration Backwards
All implants should be planned based on the final restoration. Radiographic imaging—especially CBCTs—should relate directly to the guides you’re using. Guesswork isn’t good enough.
You don’t need the latest digital intraoral scanner to do this. A denture with a radio-opaque tooth before the x-rays, converted into a guide, can be nearly as effective.
Habit 3: Guided Surgery Is No Longer Controversial
Guided surgery is definitively more accurate than freehand placement. The closer you get to fully guided, the better. Good planning at the beginning prevents amplified mistakes later. Your lab will thank you, and your implants will suffer less inflammation and infection.
Do not accept poor-quality guides from a lab—no matter how experienced they claim to be. A guide that isn’t stable is stressful and poor value. And having a guide is not a defence for poor placement.
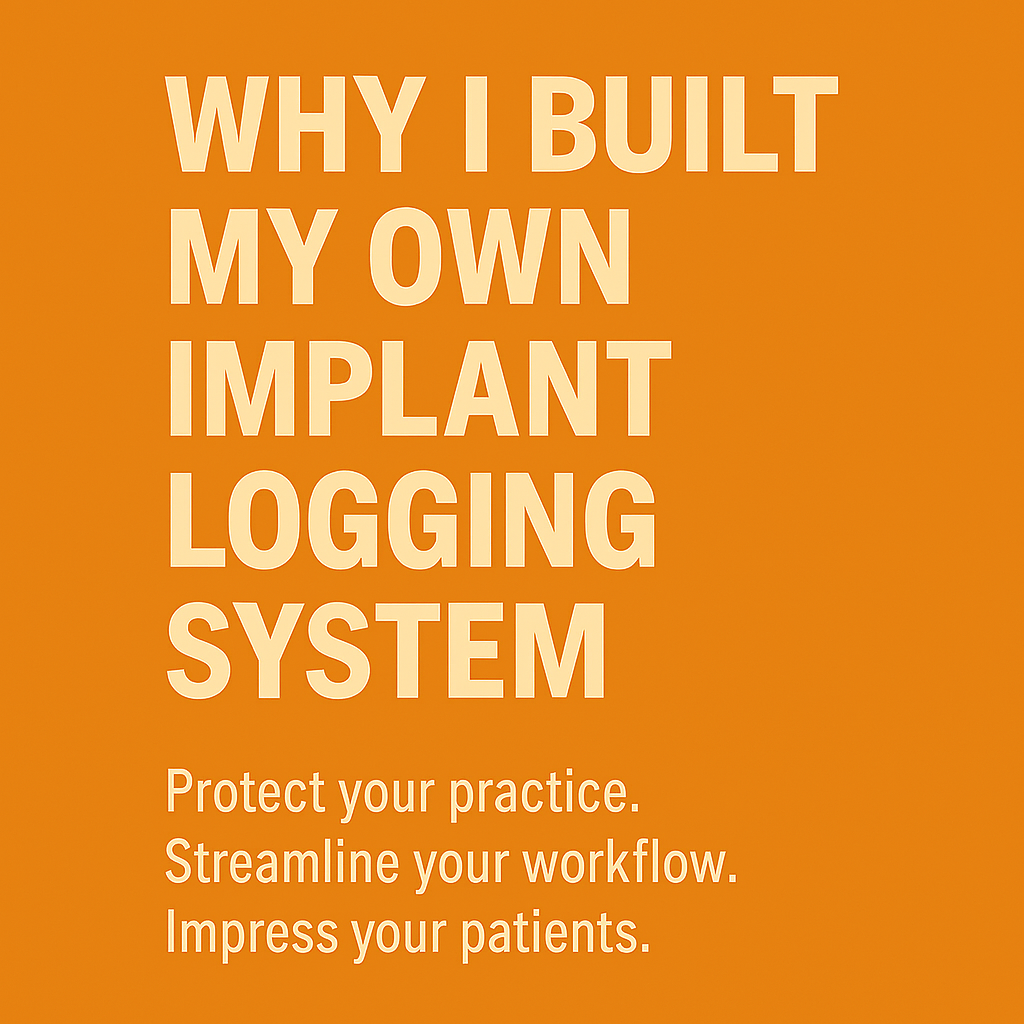
Habit 4: Keep a Log—Or Don’t Place
If you’re not keeping a log of treatment—including types, makes, and serial numbers of implant hardware—you shouldn’t be placing. It’s your moral duty to ensure the product is traceable and replaceable with minimal stress. That includes choosing suppliers who won’t vanish overnight.
Habit 5: Follow-Up Is Your Responsibility
Checking that the patient is maintaining their implants is your responsibility—even if you delegate it. Referrers and auxiliaries need to know what failure looks like and report it early.
Habit 6: Audit and Reflect Honestly
Audit your success annually—or per implant. It’s the only way to improve your technique. “Sharpening the saw,” as Covey would say, requires total transparency and honest self-reflection.
Habit 7: Mentoring Starts with a Foundation
Whenever someone asks me about mentoring, I want to know these principles are already in place. They’re the minimum standard for implant treatment. Without them, we’re not building—we’re guessing.
Whenever someone asks me about mentoring I like to know that the above principles are in place before we start, I think they have to be regarded as the basic minimum when it comes to implant treatments.
ID Blog